8 June, 2021
Would you trust healing trend data based on measurement error rates of up to 44%?[1][2]. Accurate wound measurement and valid healing trends are vital for informed decision-making and risk management.
The expectations of the changing healthcare landscape cannot be met without accurate wound measurement information, precise trend data, and thorough and consistent documentation. Find out more on the perils of manual wound measurement and the true cost of inaccuracy in the workplace.
What Is Wound Measurement?
Wound measurement is a clinical assessment process of determining the size, depth, and nature of a wound. This process includes inspection, measurement, images, and detailed documentation of each patient’s wounds.
Wound measurement is an ongoing process requiring precision and care. Measurements are taken over time at regular intervals to measure any changes to the wound (enlargements, reductions, or appearance). This information is used to aid in the treatment process, provide consistency across multiple providers, and also give estimates that can be used to predict wound healing trends accurately.
There are two main methods of wound measurement manual and digital. Manual methods rely on the examiner’s accuracy and knowledge, while digital methods provide unbiased, more accurate measurements and documentation. See here for more on manual and digital wound measuring techniques.
Why Is Wound Measurement So Important?
Current estimates expect chronic wound prevalence to grow at 8.4% per year. Accurate wound measurement and valid healing trends are vital to improving informed decision-making and better risk management in this often overlooked area of healthcare.
Imprecise measurement, poor communication, and incomplete documentation all lead to increased exposure to adverse consequences – for the patient and the organization. Wound care is becoming more accountable – underpinned by the need for evidence of healing outcomes and quality wound care practices – new demands from health policy are growing as emphasis shifts from fee-for-service to pay-for-performance funding.
Providers are now expected to meet quality indicators associated with hospital-acquired pressure ulcers, readmissions, amputations, documentation standards, and patient satisfaction. These expectations cannot be met without highly accurate wound measurement information, precise trend data, and thorough, consistent documentation.
Area And Depth – Key Metrics
While there are generally accepted standards for characterizing and assessing wounds and, consequently, measuring and reporting progress towards healing, there are several fundamental metrics; here are the two main ones.
Area Reduction Over Time
The most fundamental and often quoted metric for measuring and reporting wound healing progress is that of area reduction over time. Because this metric is used for basic evaluation of a wound’s progress[3], it is frequently used to evaluate the effectiveness of wound care processes and practices and is becoming an important determinant of reimbursement.
Reduction In Wound Volume
Another indicator used increasingly in wound measurement is the reduction in wound volume or changes in depth. This is a more difficult metric to track accurately and is becoming especially important in a litigation context.
Why Is Manual Wound Documentation So Difficult To Manage?
Wound documentation and information management are complex and variable processes that are often not given enough organizational attention. Current manual wound assessment methods are typically inaccurate – particularly in more extensive wounds where inter and intra-rater variability is high.
6 Common Issues Of Manual Wound Assessment
Wound measurement and the tracking of healing progress is a complex, variable process that is commonly affected by the following:
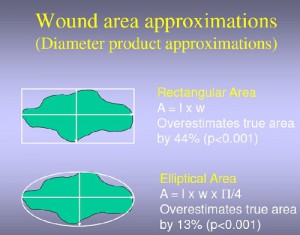
- Wounds are usually measured using fundamentally inaccurate, inconsistent, and inefficient techniques such as rulers and probes. These can introduce errors of as much as 44%.[2]
- While there may be a record of assessment, there is not sufficient information captured to show the process of assessment which would enable second opinions, audit trails and remote specialist input. [4]
- While many providers are using digital photography, the process of capturing, storing, uploading, and linking digital photographs to EMRs or paper records is unwieldy and error-prone, with poor quality photographs exacerbating risks.
- Inadequate documentation causes rework, reporting delays, and inaccuracies.
- Wound care specialists are stretched and often rely on the assessments of unskilled generalist staff.
- Poor wound documentation means that providers often pay unnecessarily high costs for wound treatments or cannot correlate treatments to healing outcomes.
The True Cost Of Inaccurate Wound Measurement
Inaccuracy, Inconsistency, and Inefficiency; are the “three i’s” that plague effective wound documentation for medical organizations worldwide.
As the focus on managing health care costs continues to intensify, funders and insurers demand more and more precise evidence of care. It is critical to have high-quality wound documentation that primarily addresses the clinical risks associated with wound care, but also provides the necessary documentation to manage legal and financial risk.
3 Types Of Wound Assessment Inaccuracy Costs
True chronic wound care costs are often hidden. The actual costs of inaccurate wound assessment can be calculated in terms of lost revenues, penalties, costs of inappropriate or ineffective treatments, and lost productivity if tasks must be repeated due to inaccurate, inefficient, and inconsistent wound assessments.
-
Direct Costs
- Lost Productivity. Due to wound re-assessment repeat work;
- Reimbursements. Repayments required due to inaccurate assessments;
- Penalties. Paid due to hospital-acquired pressure ulcers (HAPU)or lost reimbursements;
- Opportunity Costs. Due to bed days lost due to HAPU;
- Readmission. Wound-related readmission penalties;
- Litigation. Legal settlements relating to improper documentation or care.
- Inaccurate Treatment Methods/Products. The number and cost of inaccurate wound staging that could have been avoided with better measurement, imaging, trend data, monitoring, specialist reach, or expert supervision.
-
Risk Of Loss
- Duty Of Care. What is the extent and cost of wound-related errors in the organization?
- Responsibility. To what extent can your organization prove pressure ulcers were not acquired at your facility?
- Exposure. What is your organization’s exposure to wound-related litigation?
- Training. How accurate is the wound assessment capability of non-specialist nursing staff? Are the facility’s wound specialist/s overwhelmed with work? What risks are associated with these issues?
- Consequences. What would be the consequences of audit failure in wound care?
-
Lost Opportunities
- Could the facility leverage its leadership in demanding accurate wound surveillance?
- How would treatment outcomes improve if multi-disciplinary teams had instant, precise wound-healing data, imaging, and documentation at their fingertips?
- To what extent can your organization prove wound healing outcomes and be ready for pay-for-performance/evidence-based reimbursement of wound care?
- What difference would it make if patients could see their wound healing progress and the consequences of non-compliance?
- What are the current logistical costs associated with wound care? What value could be placed on a more streamlined and accurate process?
- What telehealth and other opportunities are available for wound care if assessments could be accurately measured, documented, and reviewed remotely?
Financial Consequences Of Poor Wound Management
In general clinical practice today, traditional wound measurement techniques are often cumbersome and inaccurate – introducing errors of as much as 44%[2]. As the focus on managing health care costs continues to intensify, such imprecision exposes healthcare organizations to risks and adverse financial consequences.
Litigation And Documentation Penalties
Providers are being increasingly asked to take responsibility for wound care outcomes, particularly in the area of hospital-acquired pressure ulcers (HAPU). But many are not set up to manage an increasing wound documentation burden or provide evidence of healing outcomes. They are also losing opportunities to save on wound care costs and reduce rework because they do not have the right systems in place.
In the US, for example, up to 20% of all claims and more than 10% of settlements are wound-related [5], and there are more than 17,000 pressure ulcer-related lawsuits filed annually [6]. Settlements average $250,000 [7].
There is often no cap on damages awarded where neglect can be proven in the case of pressure ulcers. And documentation is a critical success factor in pressure ulcer litigation: If documentation can prove no negligence occurred, a lawsuit is less likely to proceed. Out-of-court settlements have been forced on providers because of a lack of evidence of care, not necessarily the absence of care itself.
Continuing with the US as our example, documented demonstration of wound progress is also becoming increasingly important to payers as a determinant of reimbursement. CMS Recovery Audit Contract (RAC) audits are regularly undertaken to recoup overpayments, with wound care contributing to an estimated fee-for-service error rate of 8.5%. In 2012, 61% of the 1500 claims audited for improper Medicare payments contained errors.[8] Chronic wound prevalence has an estimated 8.4% per year growth rate, while reimbursement restrictions only intensify.
How Silhouette® Can Help
The Silhouette product suite is an innovative, non-contact, wound measurement, imaging, and documentation system that captures 3D surface topographic information about the wound and surrounding anatomy and creates a three-dimensional model of the wound, along with medical imaging and documentation.

Top 5 Benefits Of Silhouette
Wound specialists can use Silhouette to provide feedback to generalist staff to improve organizational wound care capability, and Silhouette can provide information to support second opinions and interdisciplinary care of chronic and complex wounds – read on to find out more of the benefits of the Silhouette Suite!
1. Near Perfect Accuracy
According to a statistical modeling study completed by statistician Professor Chris Frampton and ARANZ Medical’s Chief Medical Officer Dr. Mark Nixon – in order to achieve 95% confidence in wound classification at four weeks from documented healing measurements, 95% accuracy in the measurement method is required.
Silhouette measurements are highly repeatable and consistent. Inter- and intra-rater variability has been shown to be <1% for area and perimeter, and <2% for average depth and volume. Any single measurement is likely to be within approximately 2% for area, 1% for perimeter, and 5% for average depth and volume of the measured average 95% of the time for the size of wounds that have been modeled in this wound measurement accuracy study. This indicates that repeated measurements over time, even by different raters, will detect small differences as the wound changes in size and dimensions.
2. High-Quality Documentation and Reporting
Silhouette tracks healing progress and addresses documentation inadequacies from the point of care assessment through to monitoring, reporting, and auditing, and all the way to the management table where informed decisions relating to resourcing, risk, and cost management need to be made.
3. Advanced 3D Imaging
Unlike two-dimensional digital-camera planimetry methods of image measurement, which assume a wound is flat, the 3D electronic system can account for the curvature of the human body and the three-dimensional nature of wounds to derive accurate area, depth, and volume measurements.
4. Increased Usability and Accessibility
The wound measurements recorded in the Silhouette system are also able to be graphically expressed in objective wound healing trend data. The system can be integrated with EMR/PACS and is accessible to authorized remote stakeholders across the network. It can be deployed as a telemedicine solution.
5. Specialist Friendly
The electronic data provided by Silhouette improves wound-related communication for care teams and enables timely specialist input. Quality indicators can be readily tracked for reporting and audit purposes, and accurate healing rate trend data enable better-informed decisions about chronic wound management. Silhouette assists with wound surveillance, enables better detection of wound deterioration, and supports timely specialist intervention.
Silhouette Suite Components
Silhouette addresses the challenges of traditional wound measurement and information management in one easy-to-use package that can be used in a standalone or enterprise context.
- SilhouetteStar™ – a specialist scanner that captures wound images and non-contact 3D measurements of wounds and skin conditions at the point of care. The images and data captured with SilhouetteStar are uploaded to SilhouetteCentral either over a secure Wi-Fi network (SilhouetteStar 2 only) or via USB cable and SilhouetteConnect.
- SilhouetteLite+ – SilhouetteLite+ is comprised of an Application and a range-finding Sensor for Apple® iPhone® and iPad® iOS devices. SilhouetteLite+ enables users to take wound and skin images, obtain non-contact 2D measurements, and record patient notes on their Apple device. The data collected at the patient’s bedside is synchronized with SilhouetteCentral over a secure connection when available.
- SilhouetteLite – SilhouetteLite is an Application designed for Apple® iPhone® and iPad® iOS devices. SilhouetteLite is a simplified application that enables users to add patients, wound and skin images, and simple notes (without measurements) to SilhouetteCentral. The data collected at the patient’s bedside is synchronized with SilhouetteCentral over a secure connection when available.
- SilhouetteCentral™ – SilhouetteCentral is a database that stores wound and skin assessment data. It enables users to review, report, securely share and analyze the wound data collected by SilhouetteStar, SilhouetteLite+ and SilhouetteLite Applications. SilhouetteCentral is accessed via a web-based application.
- SilhouetteConnect™ + SilhouetteStar™ – SilhouetteConnect is the software installed on a Windows tablet, laptop or desktop computer. SilhouetteStar connects via USB to the computer with SilhouetteConnect installed, enabling wound and skin assessments to be performed without connection to a network. The data is synchronized with SilhouetteCentral when a network connection is available.
Contact ARANZ Medical to find out more about how Silhouette could help your skin and wound care management and give you the confidence that comes from knowing your records are accurate, consistent, and gathered efficiently.
References
- Mastronicola, D. MD and Romanelli M. MD, PhD: Clinical and Instrumental Assessment of Pressure Ulcers. Science and Practice of Pressure Ulcer Management, Springer-Verlag London Limited, 2006 pp 91-98
- Romanelli, M. MD, PhD: Wound Assessment: clinical and instrumental (presentation) (2006)
- Rodgers LC, Bevilacqua NJ, Armstrong DG, Andros G. (2010). Digital Planimetry results in more accurate wound measurements: a comparison to standard ruler measurements. J Diabetes Sci Technol. Jul 1; 4 (4) pp. 799-802.
- Putting patients first, Wounds UK 2011 Vol 7:3
- Henderson, Today’s Wound Clinic, October 2012
- AHRO ‘Preventing Pressure Ulcers in Hospitals: A Toolkit for Improving Quality of Care’
- Pressure Ulcer Resear ch: Current and Future Perspectives, 2010 Dan L. Bader et al
- US Department of Health and Human Services: Supplementary Appendices for the Medicare Fee-for-Service 2012 Improper Payment Rate Report, p 50. Table K2: Claims in Error, DME.