9 May, 2016
A statistical study modeling 120,000 wound assessments has shown that in order to achieve 95% confidence in wound classification at four weeks from documented healing measurements, 95% accuracy in the measurement method is required.
The results of the study, The Influence of Wound Measurement Precision on the Ability to Correctly Classify Wounds as “Likely Healers” or “Likely Non-Healers” at 4 Weeks, by statistician Professor Chris Frampton, and ARANZ Medical’s Chief Medical Officer Dr Mark Nixon, were presented at the recent SAWC Spring 2016 conference.
The aim of the study was to determine the relationship between the degree of precision in wound measurement and the ability to correctly classify wounds as “likely healers” and “likely non-healers” at four weeks.
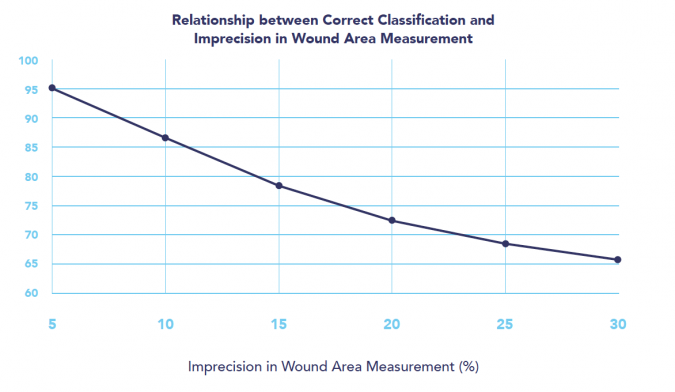
Figure 1: Graphical representation of the relationship between correct classification of healing and non-healing of wounds at four weeks and the imprecision in wound area measurement.
Dr Nixon says there is a growing body of evidence suggesting that the successful healing of different wound types can be predicted from wound area changes at around four weeks, as suggested in the model proposed by Sheehan et al in 2003.
The researchers assigned a wound of a known area for each modeled patient. They then calculated a second area representing the size of the wound after four weeks. This second area was a decrease relative to the first, chosen at random from a normal distribution (mean of 40%, standard deviation of 10%). For example, the initial area for a particular wound may have been 10cm2, and the selected percentage decrease may have been 40%, meaning a reduction in the wound area from 10 cm2 to 6 cm2.
“While the percentage reduction from 10 cm2 to 6 cm2 indicated that this patient’s wound is a ‘likely non-healer’ (i.e., it doesn’t meet the 50% threshold of the Sheehan model), the question is, how would the wound be classified if the wound was actually measured with a measurement method that contains measurement error, as all measurement methods do?” says Dr Nixon.
“For instance, instead of 10 cm2, say the initial area was measured as 12 cm2, and instead of 6 cm2 the wound at four weeks was measured as say 5 cm2. This is a measured percentage reduction of 58%,” says Dr Nixon.
“Hence the problem: At 58% reduction, the measured percentage reduction indicates that this patient’s wound is a ‘likely healer’, assuming a four-week likely healing/non-healing threshold of around 50%, whereas the true percentage reduction of 40% indicates the wound is a ‘likely non-healer’.
“So as a consequence of the limitation of the measurement method, we have incorrectly classified this wound, which can result in missed opportunities for wound healing,” says Dr Nixon.
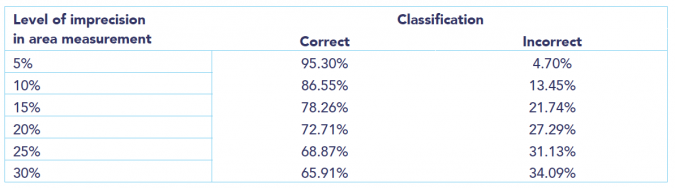
Rates of correct and incorrect classification as a function of the imprecision in wound area measurement.
For a measurement method with a particular degree of imprecision, the researchers modeled the above process for 10,000 patients, to determine how often wounds would be incorrectly classified at a particular level of imprecision. They then repeated this for six different levels of wound measurement imprecision, running a total of 60,000 simulations, which, with two assessments per wound, is equivalent to 120,000 wound assessments.
For the population modeled, the study showed that it is necessary to have 95% precision or more in wound measurement in order to correctly classify wounds 95% of the time as “likely healers” or “likely non-healers” at four weeks. Some wound measurement devices offer this level of precision.
Validating medical necessity for non-healing wounds
“The association between wound area change at four weeks and healing outcomes has a strong potential to identify patients who may need additional wound care to enable total wound healing, and those that do not,” Dr Nixon says.
This principle may be important in clinical practice, to support programs to reduce wound-related readmission, manage treatment costs, or support litigation. In clinical research, it may be important in the comparison of efficacy between different wound treatments, for instance.
Therefore, the accuracy of the measurement method used during wound assessment plays an important role in correctly assessing wound status, and getting the classification wrong can have significant wound management implications.
“Given this potential it is important to determine the role that measurement precision plays in ensuring accurate assessment of wound area change and therefore an accurate classification of likely healing or non-healing status, which was the purpose of this study,” says Dr Nixon.
Further reading:
- Download the poster (booklet form).
- Watch an educational video showing how inaccuracy in wound measurement occurs.
- Read the white paper: ‘Evidence-based wound surveillance: A three-dimensional approach to measuring, imaging and documenting wounds’.
References
Sheehan P, Jones P, Caselli A, Giurini J, Veves A. (2003). Percent change in wound area of diabetic foot ulcers over a 4-week period is a robust predictor of complete healing in a 12-week prospective trial. Diabetes Care, June 2003, 26(6): 1879-1882.