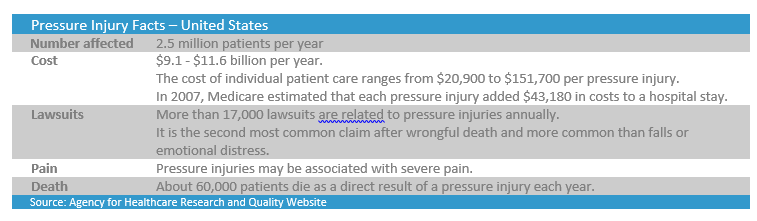
Pressure injuries are now generally considered to be preventable, but they are still a prevalent issue for many care facilities. The Agency for Healthcare Research and Quality (AHRQ) estimates more than 2.5 million people develop pressure injuries every year in the United States.
Up until the early 1900s, pressure injuries, commonly known as bedsores, were viewed as an inevitable outcome of severe illness or disability. However, now if a patient develops a pressure injury in care, it is generally considered to be an indicator of the quality of care that the patient has received. Many clinicians believe that pressure injuries can usually be prevented and, while still highly common, it is not something that should go hand-in-hand with being restricted to beds or chairs.
Despite the research and regulation that surrounds patient care, pressure injuries are still too common an occurrence that is estimated to cause the death of 60,000 patients each year in the US. Mismanaged injuries can cost tens of thousands of dollars in additional care costs for hospitals, acute care facilities, and nursing homes. In addition to this, care facilities could face fines and lawsuits that may cost them hundreds of thousands, and sometimes millions of dollars. For patients who develop pressure injuries, the cost to their quality of life is immense, causing not only psychological stress, pain, and loss of income, but can also create a burden on their families.
Managing Pressure Injuries
Pressure injuries occur when a person’s skin has pressure on it for prolonged periods of time, and are often the result of using a wheelchair or lying in one position in a bed. Frequent repositioning, correct placement of pillows/supports and proper washing practices help to prevent the onset of pressure injuries.
Once a pressure injury has presented itself, it is important to provide appropriate care for the injury as well as measure, document and monitor the wound’s healing progress. If a wound is not monitored and measured consistently, not only is it difficult for carers to provide the right treatments at the right time but also for an organization to provide an audit trail of evidence of the care that has been provided should the need arise. Acute care facilities can face a lot more than the treatment costs if pressure injuries are not managed correctly, including litigation, penalties, and a bad reputation.
Treatment Costs
When appropriate preventative measures are in place, acute care facilities can avoid the costs associated with treating pressure injuries. However, if a pressure injury develops, the costs can mount up quickly and substantially.
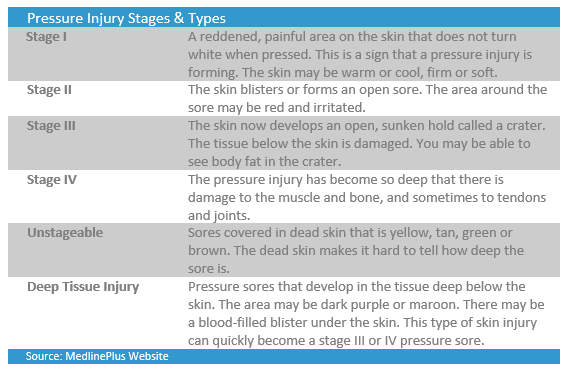
The treatment of pressure injuries costs the United States health care system between US $9 and $11 billion every year. For stage three pressure injuries, the treatment costs range between $5,900 and $14,840. Stage four pressure injuries have treatment costs that range between $18,730 and $21,410. Adding these costs on top of the treatment the patient was already receiving quickly creates a problem for the health care facilities.
Litigation Costs
As well as the actual cost of treating the pressure injury, if things were to go badly, the health care facility also opens itself up to potential lawsuits. In the United States, more than 17,000 pressure injury-related lawsuits are filed annually. Of those lawsuits, 87% settle in favor of the plaintiffs with an average settlement (for a pressure injury malpractice lawsuit) of $250,000. Yet some settlements exceed $300 million (when a wrongful death charge or class action suit is involved).
In 2015, a Tucson family was awarded $6.5 million following the medical negligence and subsequent wrongful death of their 67-year-old father. Following a stint at a Southern Arizona medical center, the man was transferred to a rehabilitation facility where he developed a pressure injury that advanced to a serious stage three as well as multiple other health problems, including malnutrition, and he ultimately lost his life.
While there are often a number of contributing factors in any pressure injury case, a lack of good quality wound documentation can seriously affect the quality of care that a patient receives, especially when there are multi-disciplinary teams caring for the patient. When there is good documentation of wounds, this can provide an audit trail that proves the quality of care that the patient has received if the case does end up in court. This article ‘The Pressure Sore Case: A Medical Perspective’ emphasizes the importance of documenting pressure injury during a trial.
Penalties
In addition to the costs of caring for the patient and potential legal costs, care facilities can also face fines or penalties for hospital-acquired infections or conditions. Medical mistakes, or “adverse events” are medical errors that healthcare facilities could and should have avoided, and are the leading cause of death in the US after heart attacks and cancer. Up to 400,000 people die each year from “adverse events” or medical mistakes in the US, which includes hospital-acquired bedsores. In California, the most prevalent adverse event across all hospitals was bedsores with 3,959 reported cases (over four years to 2014). Hospitals in California must report adverse events within five days of knowing about them or face fines.
To encourage improvements in the quality of care that hospitals provide, Medicare is changing the way it pays hospitals for services provided to people with Medicare. Instead of only paying for the number of services a hospital provides, Medicare will now also pay hospitals for providing services of higher quality and value. In addition to this, care facilities can be penalized by Medicare up to 1% of their reimbursement for a hospital-acquired, or nosocomial infection. The Affordable Care Act authorizes Medicare to reduce payments to hospitals that rank in the worst-performing quartile in the hospital-acquired condition quality measures.
Conclusion
For hospitals and care facilities, the risks associated with pressure injuries are substantial and can cost organizations thousands and in some cases even millions of dollars, not to mention the loss in quality of life for patients. With ongoing treatment costs, fines and litigation costs facing healthcare facilities, it becomes imperative for them to ensure that they are implementing pressure injury prevention programs, detecting risk factors, educating and training staff, as well as and correctly monitoring, managing and documenting any pressure injuries that do occur.
Doc Number: 2017-00165