27 January, 2016
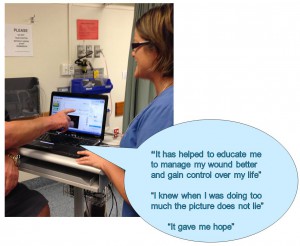
Lead author, Rebecca Aburn, consults with a patient on the healing progress of his wound using the Silhouette system.
A poster by an innovative multi-disciplinary diabetic foot ulcer clinical team has confirmed that electronic wound surveillance can improve overall patient wound outcomes.
The use of wound surveillance as an educational tool – showing patients standardized wound images and accurate wound progression graph – improves their levels of concordance and understanding, the authors have found.
The poster* shares two case studies of patients at the center.
The first was a 63-year-old male with poorly-controlled Type II diabetes whose use of Total Contact Casting (TCC) was inconsistent, leading to breakdown of his wound. Once he committed fully to the use of TCC, the wound healed. The patient reported that being able to see his wound progress via the system motivated him to “manage my wound better and gain control over my life” and gave him hope. He said the graph provided evidence of when he had taken on too much: “The picture does not lie”.
The second case was a 51-year-old male with Type II diabetes with a stage 3 pressure injury on his heel. The clinical team used the photos to encourage concordance with the treatment plan, and education about the factors leading to the wound.
The team reports that the Silhouette® system has enabled them to:
- educate, encourage and affirm wound management plans
- use objective data and remove the risk of photographic error due to images being transferred directly into the patient’s electronic health record
- collectively view overall wound progress
- predict healing peaks and troughs
- carry on with treatment plans despite setbacks.
“This system takes the guesswork out of wound management,” the poster concludes.
*Reference: Aburn, R., Schmidt, E., Van Rij, A., Krysa, J. Evidence-based Wound Surveillance Improves Practice, Concordance, and Patient Outcomes. Presented to the New Zealand Wound Care Society 7th Biennial Conference. Blenheim, New Zealand, May 2015
About the multi-disciplinary team
Putting Feet First at Diabetic Foot Clinic
Source: https://www.southerndhb.govt.nz/files/14314_20140603142718-1401762438.pdf
A multidisciplinary team based at Dunedin Hospital is at the forefront of diabetes foot care in New Zealand. The team is celebrating success in tackling the complications of diabetes which often affect diabetes sufferers’ lower limbs.
As diabetes continues to be on the increase in New Zealand, complications affecting the lower limbs are increasing. Conditions of diabetic feet can result in toe or limb amputation, a potentially devastating outcome for patients and a huge financial burden on the health service.
A weekly clinic each Friday afternoon brings together the expertise of an orthopaedic surgeon, a vascular surgeon, an endocrinologist, a wound care specialist, a diabetic nurse specialist, a podiatrist, a registered nurse and the orthotics team, enabling a comprehensive assessment and treatment plan to be sought for the benefit of the patient.
…
The team has a holistic approach to patient-centred care that includes optimal diabetes control, effective local wound care and infection control, pressure-relieving techniques and ensuring adequate blood flow to the limb. Patients are usually referred by their GPs, and once at the clinic are assessed and a treatment plan is agreed with the patient and their family.
“The team works very well and we’re one of the few clinics in New Zealand who work together as we do. We’re really seeing a difference in the outcome of patients at the clinic with this multidisciplinary approach,” commented Southern DHB Wound Care Nurse Specialist Emil Schmidt.
“An audit assessing early benefits of the clinic has shown a 50% reduction in acute admissions involving patients known to the weekly diabetic foot clinic to Dunedin Hospital over a 12-month period. Patients now have a point of contact with the clinic and we’re not seeing as many catastrophic ulcers as we used to,” he said.
Each specialist has a particular part to play in the coordinated approach:
- The orthopaedic surgeon addresses foot deformity. Correction of poorly aligned and badly functioning joints helps to heal or even prevent ulceration.
- The vascular surgeon assesses the circulation to the foot and leg.
- The endocrinologist manages the patient’s diabetes by prescribing insulin and other medications and keeps a close watch on blood sugar levels.
- The wound care specialist and the registered nurse provide patient education, support and carry out wound cleansing, removal of dead tissue and bone and formulate a wound care plan. They also work very closely with the district nursing team.
- The diabetic nurse specialist provides diabetes education and support, overseeing patients’ blood glucose levels, diabetes equipment and lifestyle, including diet.
- The podiatrist performs appropriate screening, treatment and education of diabetic patients to help prevent diabetic foot ulcers and amputation.
- The orthotics team design, fabricate and fit orthoses to relieve pressure, prevent and correct deformity and stabilize or immobilize the foot as required.
As well as the diabetic foot clinic at Dunedin Hospital, monthly wound clinics are also held across the Otago district, led by Southern DHB Nurse Specialist Wound Care Emil Schmidt, enabling patients to be managed in their home towns while receiving expert care.
Doc #2015-00596